About the Care Improvement Research Team

The Care Improvement Research Team focuses on research embedded in clinical practice. Research scientists partner with frontline clinicians to identify research questions that are important to patients and health professionals.
CIRT investigators bring rigor and scientific expertise to the process of improving clinical quality, access, and affordability while clinical partners keep the focus on the burning issues of real-world practice.
For more information, please contact us at CIRT-Group@kp.org.
Co-leadsBechien Wu, MD, MPH Program ManagerNirupa Ghai, PhD, MPH Administrative CoreAmy Vo, MBA Analytics/Biostatistics CoreErnest Shen, PhD |
CIRT Project types
Priority will be given to topics that address organizational quality goals in cardio-metabolic health, cancer care, maternal health and mental health. Health equity and telehealth are also priorities across these quality domains.
| CIRT Project Type | Budget and Time Frame | Review/Considerations |
| Planning projects to develop project proposals through engagement and discovery with regional clinical leaders | 4 projects: up to $10K, < 3 months, per project |
|
| Rapid cycle data-only care delivery/program evaluation projects to inform time-sensitive clinical-operational decision making that require advanced statistical analyses | 4 projects: up to $50K, 3-12 months per project |
|
| Pilot care delivery program implementation and mixed-methods evaluation projects to inform clinical and operational decision-making. | 2 projects: up to $150K, 1-2 years per project |
|
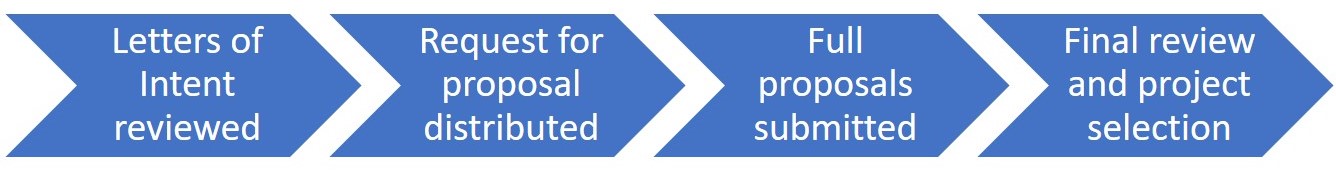
2025 CIRT Proposal Review Process
CIRT project awards range between $10,000 and $150,000 (over two years) per proposal, and aim to improve quality, affordability, wellness, and equitability. Funding support is generally available for one year. The CIRT team releases a request for proposals annually. The timeline for 2026 proposals is:
- Letter of Intent announcement: July 28, 2025
- Letter of Intent due: August 29, 2025
- Request for full proposals: October 6, 2025
- Full proposals due: November 13, 2025
- Earliest project Start date: Quarter 1 2026
Eligibility criteria
Any employee of the Department of Research & Evaluation, or any physician associated with SCPMG is eligible to submit a CIRT project proposal. Directors of each division (Behavioral, Epidemiology, Health Services, Clinical Trails) and the Chair of the Regional Research Committee are eligible to nominate at least one CIRT project. Non-scientific staff should identify a scientist or experienced physician investigator to serve as a Co-Principal Investigator and project mentor.
Submission examples
To learn the details of what is required in submission applications, you can read the examples below.
Project timeline
CIRT projects are considered rapid-cycle projects. Funding is generally available for one year of support. It is highly recommended that all study-related activities, including analysis, be completed in the 12-month funding period. Funding extensions will be submitted to the executive sponsors for approval on a case-by-case basis.
For more information, please contact us at CIRT-Group@kp.org.
The Care Improvement Team is now supporting the following projects in 2025:
Cardiac rehabilitation disparities, challenges, and opportunities in Kaiser Permanente Southern California
Leads: Matthew Mefford, PhD; Columbus Batiste, MD; Debora Lahti, MSN; Tadashi Funahasi, MD; Rachid Elkoustaf, MD, MPH; Chileshe Price, MD
Mental health at Kaiser Permanente Southern California: outcomes of feedback informed care
Leads: Laurel Sarfan, PhD; Elizabeth Hamilton, LCSW, MPH; Khadijah Bhutto Ramirez, PsyD, LMFT; Nicole Corey, LMFT; Ryan Nguyen, MPH
E-surveillance of outpatient safety risk (SureNet)
Leads: Tracy Imley, MD; Karen J. Coleman, PhD
Advanced practice providers in urgent care
Leads: Jarlath Ryan, MD; Amy Wolf, MD; Thearis Osuji, MPH; Bechien Wu, MD
Evaluation of Abridge implementation
Leads: Eugene Chu, MD; Karen J. Coleman, PhD
Diabetes control in Latine members
Leads: John Martin, MD; Taynara Formagini, PhD; Karen J. Coleman, PhD; Bechien Wu, MD
Individuals experiencing or at risk for homelessness
Leads: Kaiser Permanente Southern California Medi-Cal Team; Claudia Nau, PhD
Asthma home remediation
Leads: Kaiser Permanente Southern California Medi-Cal Team; Corinna Koebnick, PhD
These are newly funded projects as of July/August 2025:
Comparative outcomes of heart failure patients following acute care hospitalization and advanced medical care at home
Leads: Cheng-Wei (Charlie) Huang, MD, FACP; Huong Nguyen, PhD, RN; Bing Han, PhD; Mingsum Lee MD, PhD
Atrial fibrillation care pathway in KPSC (VTAC: Virtual Total Arrhythmia Care)
Leads: Nigel Gupta, MD; Teresa N. Harrison, SM; Mercedes Munis, MPH; Kevin Stiles, MD; Timothy Ho, MD, MPH; Ray Nanda, MD; Kim-Huong Tran, MD; William Woo, DO; Ronald Loo, MD; Jonathan Finkelstein, MD, MPH; Columbus Batiste, MD; Mingsum Lee, MD, PhD
Pancreas cancer early detection for surgical oncology referral program
Leads: Bechien Wu, MD, MPH; Victoria O’Connor, MD; Dan Zisook, MD; Douglas Murad, MD
Effectiveness of a systematic approach to care for patients with Lynch syndrome
Leads: Bechien Wu, MD, MPH; Monica Alvarado, MS, LCGC; Trevor Hoffman, MD, PhD
Collaborative Planning to Support Postpartum Mental Health at KPSC
Leads: Laurel Sarfan, PhD; Corinna Koebnick, PhD; Sonya Negriff, PhD; Khadijah Bhutto Ramirez, PsyD, LMFT; Gloria Martinez, LMFT, RPT-S; Leigh Miller, LSCW
2024
GLP-1 use and anesthesia risk
Leads: Chunyuan Qiu, MD, MS, and Bechien Wu, MD, MPH
Social risk screening and intervention
Leads: Tim Ho, MD, MPH, and Thearis Osuji, MPH
Effectiveness of advanced practice providers in urgent care
Leads: Jarlath Ryan, MD, and Thearis Osuji, MPH
Optimal NICU surveillance time post-acute cardio-pulmonary events
Leads: Nicholas Lynch, MD; David Braun, MD; and Thearis Osuji, MPH
Improving patient safety: Optimizing systems to save lives (SureNet)
Leads: Tracy Imley, MD, and Karen J. Coleman, PhD, MS
Understanding factors related to diabetes control in Latin(e) members
Leads: John Martin, MD and Karen J. Coleman, PhD, MS
Impact of the Abridge AI tool on physician practice and patient satisfaction
Leads: Eugene Chu, MD, and Karen J. Coleman, PhD, MS
Medi-Cal: Medically tailored meals
Lead: Karen J. Coleman, PhD
Medi-Cal: Enhanced care management and supports for homeless members
Lead: Claudia Nau, PhD
Medi-Cal plus other programs to improve birth equity
Lead: Heidi Brown, MD, MAS
Medi-Cal: Asthma home remediation
Lead: Corinna Koebnick, PhD, MSc
Medi-Cal/Medicare: PACE for members at risk for institutionalization
Lead: Huong Nguyen, PhD, RN
2023
Therapeutic intensification for uncontrolled hypertension
Principal investigator: Jaejin An, PhD, Division of Epidemiologic Research
Improving computerized clinical decision support alerts
Principal investigator: Lewei Duan, PhD, MS, Division of Health Services Research & Implementation Science
Systematic evaluation of KPSC peer-to-peer (P2P) support programs
Principal investigators: Thearis Osuji, MPH, Division of Health Services Research & Implementation Science, and Kerry Litman, MD
Immediate post-placental intrauterine device insertion: Comparative analysis of outcome measures including complication rates and effects on reproductive life planning
Principal investigator: Asma J. Saraj, MD
Effect of a pharmacist-led multipronged educational intervention on benzodiazepine and sedative-hypnotic drug prescribing among ambulatory adult patients
Principal investigators: Steven Steinberg, MD, Patricia Gray, PharmD
Evaluation of a remote blood pressure monitoring program for hypertension management
Principal investigator: Kristi Reynolds, PhD, Division of Epidemiologic Research
Increasing pediatricians’ provision of digital self-care tools to adolescents (ages 13 to 17) with mild-to-moderate depressive symptoms
Principal investigator: Davida Becker, PhD ScM
Observed role of cooling on hemodynamics in inpatient dialysis (ORCHID), continuation
Principal investigator: Hui Xue, MD, MMSc
The initiation of guideline-directed medical therapy during hospitalization for congestive heart failure patients and its impact on post-discharge outcomes, continuation
Principal investigator: Cheng-wei Huang, MD
Prevalence, trend, care delivery and disparity in mental health conditions in children, adolescents, and young adults among KPSC members, continuation
Principal investigator: Anny Xiang, PhD, Division of Biostatistics Research
Improving care transitions and reducing readmissions: Medically tailored meals for Medi-Cal members, continuation
Principal investigator: Huong Nguyen, PhD, RN, Division of Health Services Research & Implementation Science
Implementation and evaluation of an enhanced Adverse Childhood Experiences (ACEs) screening and referral system in pediatric primary care, continuation
Principal investigator: Sonya Negriff, PhD, Division of Behavioral Research
Venous thromboembolism prevention in abdominal surgical patients with cancer, continuation
Principal investigator: Michael K. Gould, MD, MS, Kaiser Permanente Bernard J. Tyson School of Medicine
Implementing systematic distress screening in medical oncology, continuation
Principal investigator: Erin E. Hahn, PhD, MPH, Division of Health Services Research & Implementation Science
Enhanced implementation of lung cancer screening, continuation
Principal investigator: Michael K. Gould, MD, MS, Kaiser Permanente Bernard J. Tyson School of Medicine





