
EIS officer makes a difference here and abroad
As an Epidemic Intelligence Service officer with the Centers for Disease Control and Prevention, Lisa Oakley, PhD, MPH, knew she would have an excellent training experience using electronic health records to find answers to important clinical and public health questions when she reported to the Kaiser Permanente Southern California Department of Research & Evaluation in 2018.
But in addition, she found herself in Ghana, North Dakota, and at the heart of the early response to the coronavirus pandemic in Seattle. Then she was back in the department’s Pasadena headquarters, assisting Kaiser Permanente’s national response to the coronavirus.
“My expectation coming in was that the majority of my time would be working on Kaiser Permanente research projects in Southern California and then I would have 1 or 2 field experiences with the Los Angeles County Department of Public Health,” Dr. Oakley said. “Instead, I had field experiences I never could have expected.”
EIS program responds to public health emergencies
The EIS program is a competitive 2-year fellowship that combines applied, on-the-job learning with service. EIS officers are the first-line rapid responders for conducting outbreak investigations, surveillance, and public health responses for the CDC. They are often referred to as “disease detectives.”
“The most pop culture reference I’ve used for friends and family is that I was basically Kate Winslet’s character from the movie Contagion,” she said. “The character was actually based on the CDC’s Principal Deputy Director and EIS alumna, Anne Schuchat, MD (RADM, USPHS, RET). Dr. Schuchat was a keynote speaker at last year’s American College of Epidemiology meeting, which was hosted by the Department of Research & Evaluation.
About two-thirds of EIS officers are stationed at the CDC headquarters in Atlanta, while the others are stationed elsewhere throughout the United States. Dr. Oakley was the second EIS officer stationed at the Kaiser Permanente Department of Research & Evaluation. Gloria Chi, PhD, MPH, was the first EIS officer assigned to R&E, in 2016.
EIS alumnae at KP act as mentors
In the Department of Research & Evaluation Division of Epidemiologic Research, Dr. Oakley’s primary mentors were 2 EIS alumnae Jean Lawrence, ScD, MPH, MSSA, and Sara Tartof, PhD, MPH, as well as Senior Director of Research Steven J. Jacobsen, MD, PhD. (She completed her program in late June, 2020.)
Dr. Oakley earned her PhD in Behavioral Sciences and Health Education from Emory University in Atlanta, her MPH in International Health from Oregon State University in Corvallis, Oregon, and her BA in philosophy from Willamette University, in Salem, Oregon.
“I was attracted to the Kaiser Permanente position because of the ability to do important research and then have the opportunity to have the findings translated back into the health system, positively affecting the lives of Kaiser Permanente members,” she said. “And that felt like the epitome of public health: the ability to take what we’re learning and improve people’s health and well-being.”
Variety of responses was unexpected
Dr. Oakley arrived at R&E in 2018, expecting to spend most of her 2 years in the office.
 “It had been a quiet couple of years in terms of major disease outbreaks, so the EIS program had tempered our expectations regarding responding to major events,” Dr. Oakley said. “And so, I thought that my field experiences would be with the Los Angeles County Department of Public Health.”
“It had been a quiet couple of years in terms of major disease outbreaks, so the EIS program had tempered our expectations regarding responding to major events,” Dr. Oakley said. “And so, I thought that my field experiences would be with the Los Angeles County Department of Public Health.”
In February and March 2019, she was called upon to assist the California Departments of Health and Education in a statewide investigation into the use of electronic cigarettes in California high schools. She immediately followed that investigation with another in Pennsylvania to assess the quality of data being gathered about opioid-associated neonatal abstinence syndrome, a condition that occurs in newborns who are exposed to opioid drugs while in their mother’s womb.
A few months later, after she had returned to California, information came out that use of e-cigarettes, also known as vaping, was associated with an outbreak of lung injuries. Dr. Oakley was tasked with co-leading the development of the response plan for the Los Angeles County Department of Public Health.
Responding to e-cigarette outbreak
“I provided the public health department with technical assistance on e-cigarettes, updated them on the current public health knowledge on the emerging outbreak, and developed a plan for assessment and investigation of the e-cigarette-associated lung injuries reported to the health department,” she said.
Dr. Oakley also assisted in the training of over 100 public health nurses on e-cigarette products and a protocol for patient interviews and specimen collection.
At the beginning of this year, she responded to a poliovirus outbreak and assisted with a supplemental immunization campaign in Ghana. She returned from Ghana in February and found herself suddenly on the front lines of the COVID-19 response. She was first sent to Seattle in early March on the weekend that the COVID-19 cluster in a nursing home hit the news.
On the front lines of the COVID-19 response
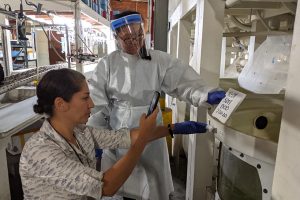
“During my 2 weeks in Seattle, I worked primarily with long-term care facilities, assisting those with current outbreaks, trying to prevent outbreaks in other facilities, and supporting the testing and prevention of COVID-19 among health care personnel,” she said. “I also helped manage a drive-through testing site for symptomatic health care workers who had been exposed to patients with COVID-19.”
 Afterward, she co-authored one article on the rapid transmission of COVID-19 in a nursing home, and another article on the epidemiology of COVID-19 in a long-term care facility. Both were published initially as brief reports in the CDC’s Morbidity and Mortality Weekly Report and later in the New England Journal of Medicine.
Afterward, she co-authored one article on the rapid transmission of COVID-19 in a nursing home, and another article on the epidemiology of COVID-19 in a long-term care facility. Both were published initially as brief reports in the CDC’s Morbidity and Mortality Weekly Report and later in the New England Journal of Medicine.
Then in April, she spent 2 weeks in North Dakota, serving as the infection prevention and control lead for the CDC team sent to aid in the North Dakota Department of Public Health’s COVID-19 response. While in North Dakota, she responded to an outbreak at a wind power factory, developed a comprehensive testing strategy, and assisted the health department in developing and updating guidance for adult care homes and workplaces.
Using EIS experiences in KP’s strategy
She returned to Pasadena in mid-April and worked with a team of national Kaiser Permanente leaders on the next phase of the organization’s COVID-19 response, until her appointment ended in late June.
“Lisa was such an outstanding contributor to these efforts to address COVID prevention; we are so grateful to her, her mentors and to the CDC for the excellent work she’s done to help us on these two major projects,” said David C. Grossman, MD, MPH, Kaiser Permanente’s national senior medical director for Community Health.
The work includes developing ways to reduce COVID-19 infections within families and households, and a monitoring system to identify potential hot spots of emerging outbreaks.
“While both of these projects are still in development, I feel lucky to have the opportunity to contribute to a broader-scale approach to COVID-19 for our members and communities,” Dr. Oakley said.
Maternal health became research topic
Among the research Dr. Oakley is most proud of is a study she conducted with Dr. Lawrence and Dr. Tartof on race and ethnic disparities in maternal health outcomes. She investigated racial/ethnic disparities in the trends of severe maternal morbidity during delivery hospitalizations at Kaiser Permanente Southern California hospitals from 2008 to 2017. Severe maternal morbidity includes severe unexpected outcomes of labor and delivery such as sepsis, acute heart failure, eclampsia, and hysterectomy that can result in significant short-or long-term consequences to a woman’s health.
In the United States, rates of severe maternal morbidity have increased over the last 15 years. Women of color, and particularly black women, are at increased risk of experiencing severe maternal morbidity and mortality.
Dr. Lawrence said that one of the primary reasons she and Dr. Tartof selected Dr. Oakley to be the department’s EIS officer was her interest in health disparities and maternal and child health.
“I have studied disparities in gestational diabetes and other complications of pregnancy but had not examined severe maternal morbidity. We thought it was essential to look at this important outcome of pregnancy among our patients,” Dr. Lawrence said. “Consistent with other studies, we found that black women are at the highest risk of severe maternal morbidity while other women of color also had a significantly higher risk than non-Hispanic white women.”
The researchers also are working with 2 Southern California Permanente Medical Group physicians—an obstetrician who specializes in high-risk pregnancies, and a family medicine physician who is the co-lead of the SCPMG Equity, Inclusion and Diversity Team—to better understand the potential causes of these disparities and consider how to best address them.
 Dr. Oakley has been a good ambassador
Dr. Oakley has been a good ambassador
Dr. Tartof said that during her time with Kaiser Permanente, Dr. Oakley shined a bright positive light on the organization through her research and her leadership.
“Lisa did a tremendous job in so many different public health capacities and working with so many different health departments, including our own county health department,” Dr. Tartof said. “She moved seamlessly from one group to another, one situation to another, each time being very inclusive and very generous and naturally rising to a leadership position.”
Honored with health equity award
Due in part to this work, Dr. Oakley was the 2020 recipient of the Shalon M. Irving Health Equity Award given by the EIS Alumni Association for commitment to health equity and racial disparities research, Dr. Lawrence said.
The award was named in memory of Dr. Shalon Irving, an EIS alumnae who died unexpectedly in 2017, just 3 weeks after giving birth, calling attention to one of the widest of all racial disparities in women’s health, disproportionately high rates of maternal mortality among black women in the United States.
Dr. Oakley said her EIS experience was more than she could have ever hoped for.
“It was a really amazing balance of research, evaluation, and response, both domestic and international,” Dr. Oakley said. “You know, I don’t think I could have imagined a more varied EIS experience than what I’ve had.”





