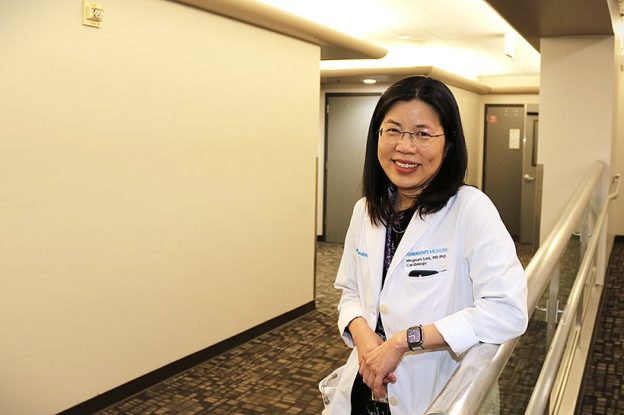
Five questions for Dr. Mingsum Lee
Mingsum Lee, MD, PhD, has been named as the 2025 Southern California Permanente Medical Group Physician Researcher of the Year. Commenting about her selection for the award, one nominator said Dr. Lee “is a true quadruple threat as an exceptional clinician, educator, administrator, and prolific researcher, but also has a humility and generosity which defines her personality.”
She serves as chief of service for the Department of Cardiology at Kaiser Permanente Los Angeles Medical Center and as the area research chair for Los Angeles on the Kaiser Permanente Southern California Regional Research Committee.
Dr. Lee’s research focuses on cardiovascular disease, particularly the evaluation of cardiovascular testing and therapies. Her work evaluates patterns of utilization and patient outcomes to improve the value of these interventions in clinical practice. She has extensive experience working with large datasets and expertise in leveraging data resources and integrating them into clinical operations to improve efficiency and enhance care quality.
She has authored more than 100 peer-reviewed publications and presented over 100 scientific abstracts at national conferences. Below she answers 5 questions, and a few bonus questions, as well.
When and where did your interest in becoming a doctor and researcher begin?
I’ve been drawn to applied science from a very young age, fascinated by how logic, experimentation, and structured reasoning can be used to solve real-world problems. The study of medicine represents some of the most complex and challenging questions in all of science, and that intellectual challenge is what initially drew me to the field. Although the science brought me into medicine, as I grow older, I’ve come to treasure the humanistic side most deeply. It is a profound privilege to be a physician — to connect with people in a deep and meaningful way and to have the opportunity to make a difference in their lives.
Practicing at Kaiser Permanente is especially rewarding because of its integrated model of care. Day to day, we care for patients one-on-one, and that individual connection is incredibly fulfilling. At the broader level, physicians also play a critical role in designing, implementing, and evaluating programs that improve care for entire populations. We use robust research methods to understand what works, refine what doesn’t, and continuously improve outcomes for our patients. This dual perspective — deeply personal patient care combined with population-level impact — makes Kaiser Permanente an exceptional place to practice medicine.
How did you come to Kaiser Permanente?
When I studied health systems in graduate school, Kaiser Permanente came up as a model that could solve many of our nation’s health care challenges. I chose to work here because I wanted to see firsthand how this system functioned in real life, and what I discovered was even better than I expected.
Over the past 10 years, I’ve found that Kaiser Permanente is far more than a well-functioning health system that delivers true population care. It is a community of people who are kind, compassionate, and deeply mission driven. What I appreciate most is that our leaders never lose sight of our true north: the patient. Every decision and every initiative ultimately returns to what is best for the patients we serve. I am grateful every day to be part of a community of physicians who genuinely care about their patients and about one another.
When did you become involved in research at Kaiser Permanente?
Like many physicians at Kaiser Permanente, I am a front-line physician and spend most of my time caring for patients. As physicians, our primary responsibility is to ensure that our patients receive the best care possible. However, being a physician can be profoundly humbling.
No matter how much we study, there will always be things we do not know.
There are rare diseases, unusual presentations of common conditions, and an ever-growing body of medical knowledge. Despite our best efforts and all the advances in medicine, there are still moments when we walk into a patient’s room and have to tell families that we don’t have all the answers, that the evidence is incomplete or simply does not exist. Those moments can be heartbreaking, but they can also be motivating.
They remind us that we have both the opportunity and the responsibility to use our data and our collective expertise to help patients find answers where none currently exist. That means rigorously reviewing the latest research and, when evidence is lacking, drawing on our extensive data resources, shared clinical wisdom, and close collaborations to help guide patients toward the best possible path forward.
When and why did you start mentoring, and why is that important to you?
I served for 8 years as the program director for the cardiology fellowship, an appointment that ended in September. I continue to mentor cardiology fellows, both clinically and in their research projects. The fellowship program is an investment in our future, and my colleagues and I dedicate significant personal time and effort to building the program and working with trainees one-on-one. It is truly a labor of love.
We do this because we believe that for any health system to prosper, it must invest in its next generation of clinicians. I also believe deeply in the synergy between research, clinical care, education, and innovation. For our health system to function as a true learning health system, it must be supported by both education and research.
What research are you most proud of?
It’s hard to single out one project I am most proud of. In general, the projects that mean the most to me are those that answer a clinical question brought forward by a clinician or a patient. That philosophy guides how I choose my research questions.
For example, one of my patients had been hospitalized with a rare cardiac condition and wanted to know the likelihood of it recurring. Because the condition is uncommon, there was very little published information. The data infrastructure at Kaiser Permanente allowed us to evaluate the recurrence rate and identify associated risk factors. When I called her to share what we had learned, and to tell her that her question had inspired the project, she cried and said she was grateful to have contributed to work that might help other patients like her.
While I have worked on projects evaluating the operational impact of clinical programs that affect far larger populations, in the end, it is always the research that directly answers real patient questions that I find most meaningful and fulfilling.
What research are you working on now and why is it important?
I am working on several population-based research projects that are now possible because of advances in natural language processing and our ability to extract structured information from unstructured clinical text. I am also working on studies that leverage data from our electronic health records to identify patients at risk for cardiovascular events years before those events occur, enabling earlier intervention.
One of our greatest strengths as an integrated health system is the ability to proactively identify patients at risk and implement programs that reduce those risks before disease develops. Our technology infrastructure and electronic health record systems allow us to follow patients proactively and provide an added layer of support. Patients are cared for not only by the physicians they see, but also by a system designed to flag when surveillance testing is due, when risk factors are not optimally controlled, and when timely intervention may prevent deterioration. These initiatives are powerful and enable the system to ensure that patients receive the care they need.
What do you enjoy doing in your spare time?
I enjoy learning and have always loved reading. I still enjoy visiting bookstores, even though there are far fewer of them today. When I travel, I especially enjoy visiting historic libraries, and you’ll often find me wandering through the rare books section in museums.





